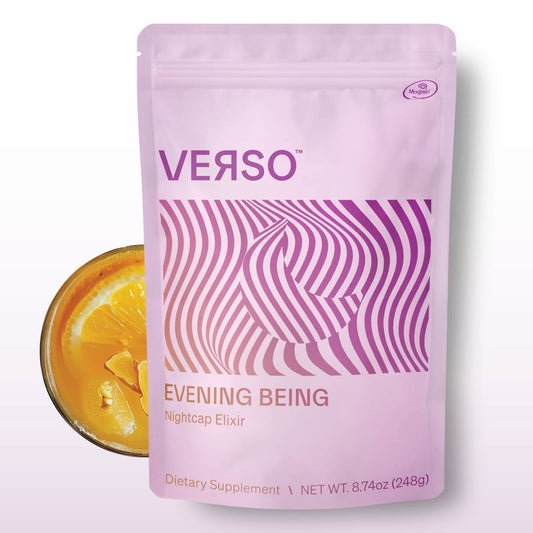
What is Luteolin?
Luteolin is a plant pigment belonging to the flavonoid family. Dietary sources include citrus fruits, broccoli, carrots, celery, parsley and oregano (1). Supplementation with luteolin is believed to confer longevity benefits. Most of the research that exists on the benefits of luteolin have been in vivo (animal or organism research) and in vitro (cell research).
Effects of luteolin on oxidative stress
Oxidative stress causes cell and DNA damage; it is akin to cellular aging. Oxidative stress is an imbalance between antioxidants and free radicals or reactive oxygen species (ROS) within the cell. Since luteolin is a flavonoid, it acts as an antioxidant to control oxidative stress.
It has been noted to suppress ROS and inhibit ROS-related cellular damage (8, 9). In addition, luteolin has been noted to activate an important antioxidant gene pathway, nuclear factor erythroid 2-related factor 2 (Nrf2), which confers additional antioxidative benefits (8).
Effects of luteolin on inflammation
Chronic inflammation is directly related to the acceleration of aging and the development of diseases of aging (10). In animal studies, luteolin has been shown to prevent inflammation of the lungs, nose and brain via the inhibition of pro-inflammatory cytokines (11, 63).
In mice, luteolin also prevents viral-induced inflammation in the breast and lung (14, 15). Additionally, in various cells luteolin inhibits major signaling associated with inflammation, including Nf-kB, TLR4, and cytokine expression (12-14).
Effects of luteolin on heart health
Several studies have found that luteolin supports heart health. Studies in mice have shown that luteolin strengthens heart cells and heart contractions (2, 4). Other animal studies have found that luteolin prevents damage of heart tissues and heart cell death (3, 4).
Luteolin was also found to reduce oxidative stress-induced damage during a simulated heart attack in the isolated hearts of mice (5). Another possible heart benefit of luteolin is the prevention of atherosclerosis, via the reduction of inflammation and fat buildup in blood vessels, which has also been found in mice (6, 7).
Effects of luteolin on the brain and nervous system
Across various animal and cell studies, luteolin has been shown to have neuroprotective effects and to support nerve development. This effect is likely due to luteolin’s ability to reduce glutamate levels, suppress brain inflammation and deter oxidative stress. These benefits support hippocampal neuron growth and prevent the mutation of neural proteins (16-20).
Additionally, animal research in mice with Alzheimer’s Disease have supported this evidence (21-23). Research has also shown that luteolin ameliorates the symptoms of Alzheimer’s in mice through increasing cognition, memory and balance (21-23).
Similarly, in cell assays, luteolin has also been shown to protect human brain cells against cellular aging caused by oxidative stress and Alzhiemer’s-associated inflammation and proteins (24, 25).
Luteolin supplementation may also protect against depression. Studies in mice and cells have found that luteolin may protect nerves in the hippocampus, the brain region dedicated to emotions and memory, and also activate gamma-aminobutyric acid (GABA) receptors, associated with improved mood (26-28).
In mice, luteolin supplementation has also been shown to decrease symptoms of parkinson’s disease, multiple sclerosis, and brain trauma (29-32).
All in all, luteolin supplementation may be an effective route to suppress brain inflammation, suppress oxidative stress induced brain damage and enhance beneficial neural cell signaling pathways.
Effects of luteolin on cancer
Due to luteolin’s antioxidant properties, it is believed that luteolin can protect against cancer. Animal studies have shown that luteolin can prevent the growth of prostate, breast, lung, stomach, colon, ovarian and liver cancers (33-42).
Similarly, cell studies have found that luteolin confers protection for pancreatic and brain cancer (43-48). Research also suggests that luteolin may help to reduce drug-resistant cancer cell growth, via inducing cancer cell apoptosis, and enhance chemotherapy effectiveness (47,48).
Effects of luteolin on the immune system
Luteolin supplementation has been shown to enhance the immune system in various ways. In animal studies, luteolin blocks lipopolysaccharide-induced (LPS) inflammation which is associated with bacterial infection (49-52).
In fact, one study found that luteolin’s ability to block LPS-induced inflammation enhanced animal survival rate (52). In support of this attribute, cell studies have shown similar results (53, 54).
Luteolin has also been found to inhibit viral spread in mice, including both Epstein-Barr and hepatitis B (55-57). A cell study also supports this evidence, suggesting that luteolin has antiviral capacities against Japanese encephalitis virus (58).
Effects of luteolin on skin aging
Animal research has found that luteolin may reverse skin aging and prevent the development of skin cancer (59, 60). This effect is likely due to the antioxidative properties of luteolin, which protect the skin from sun damage.
Effects of luteolin on male hormones
For men, luteolin supplementation may also confer hormone benefits. Cell studies have shown that luteolin inhibits aromatase, which may prevent the conversion of male sex hormones into estrogen (61). In this sense, luteolin may work to boost testosterone levels.
For instance, in mice exposed to a strong electromagnetic field, luteolin boosted testosterone levels (62). However, further research is needed to investigate these effects more thoroughly.
What does this all mean?
Preclinical research on luteolin suggests that it has intriguing anti-inflammatory and antioxidant properties which may confer benefits to the heart, brain, immune system, nervous system, skin and hormones.
It also may offer protection against specific cancers. Most of the clinical trials investigating these effects in humans are still underway. The doses seen in research are doses more likely to be found in supplements as opposed to the diet.
As always, weigh the pros and the cons based on the current evidence and reach out to your physician if you’re interested in supplementation. It is advised that pregnant women, individuals with cervical cancer and children avoid supplementation with luteolin.

Author: Jacqueline Seymour
Jacki is a Master’s student at USC, home of Dr. Valter Longo’s Longevity Institute, where she’s studying her passion for life: Gerontology(the science of aging) and Nutrition.
References:
- López-Lázaro M. Distribution and biological activities of the flavonoid luteolin. Mini Rev Med Chem. 2009 Jan;9(1):31-59. doi: 10.2174/138955709787001712. PMID: 19149659.
- Wu, Xin et al. “ERK/PP1a/PLB/SERCA2a and JNK pathways are involved in luteolin-mediated protection of rat hearts and cardiomyocytes following ischemia/reperfusion.” PloS one vol. 8,12 e82957. 30 Dec. 2013, doi:10.1371/journal.pone.0082957
- Fang F, Li D, Pan H, Chen D, Qi L, Zhang R, Sun H. Luteolin inhibits apoptosis and improves cardiomyocyte contractile function through the PI3K/Akt pathway in simulated ischemia/reperfusion. Pharmacology. 2011;88(3-4):149-58. doi: 10.1159/000330068. Epub 2011 Sep 16. PMID: 21934351.
- Qi L, Pan H, Li D, Fang F, Chen D, Sun H. Luteolin improves contractile function and attenuates apoptosis following ischemia-reperfusion in adult rat cardiomyocytes. Eur J Pharmacol. 2011 Oct 1;668(1-2):201-7. doi: 10.1016/j.ejphar.2011.06.020. Epub 2011 Jun 26. PMID: 21723277.
- Zhang, R. Q., Li, D. Y., Xu, T. D., Zhu, S. S., Pan, H. J., Fang, F., Wu, X., & Sun, H. (2017). Antioxidative effect of luteolin pretreatment on simulated ischemia/reperfusion injury in cardiomyocyte and perfused rat heart. Chinese journal of integrative medicine, 23(7), 518–527. https://doi.org/10.1007/s11655-015-2296-x
- Li, J., Dong, J. Z., Ren, Y. L., Zhu, J. J., Cao, J. N., Zhang, J., & Pan, L. L. (2018). Luteolin decreases atherosclerosis in LDL receptor-deficient mice via a mechanism including decreasing AMPK-SIRT1 signaling in macrophages. Experimental and therapeutic medicine, 16(3), 2593–2599. https://doi.org/10.3892/etm.2018.6499
- Jia, Z., Nallasamy, P., Liu, D., Shah, H., Li, J. Z., Chitrakar, R., Si, H., McCormick, J., Zhu, H., Zhen, W., & Li, Y. (2015). Luteolin protects against vascular inflammation in mice and TNF-alpha-induced monocyte adhesion to endothelial cells via suppressing IΚBα/NF-κB signaling pathway. The Journal of nutritional biochemistry, 26(3), 293–302. https://doi.org/10.1016/j.jnutbio.2014.11.008
- Zou, Y., Luo, X., Feng, Y., Fang, S., Tian, J., Yu, B., & Li, J. (2021). Luteolin prevents THP-1 macrophage pyroptosis by suppressing ROS production via Nrf2 activation. Chemico-biological interactions, 345, 109573. https://doi.org/10.1016/j.cbi.2021.109573
- Yang, S. C., Chen, P. J., Chang, S. H., Weng, Y. T., Chang, F. R., Chang, K. Y., Chen, C. Y., Kao, T. I., & Hwang, T. L. (2018). Luteolin attenuates neutrophilic oxidative stress and inflammatory arthritis by inhibiting Raf1 activity. Biochemical pharmacology, 154, 384–396. https://doi.org/10.1016/j.bcp.2018.06.003
- Ferrucci, L., & Fabbri, E. (2018). Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nature reviews. Cardiology, 15(9), 505–522. https://doi.org/10.1038/s41569-018-0064-2
- Jang, T. Y., Jung, A. Y., Kyung, T. S., Kim, D. Y., Hwang, J. H., & Kim, Y. H. (2017). Anti-allergic effect of luteolin in mice with allergic asthma and rhinitis. Central-European journal of immunology, 42(1), 24–29. https://doi.org/10.5114/ceji.2017.67315
- Kao, T. K., Ou, Y. C., Lin, S. Y., Pan, H. C., Song, P. J., Raung, S. L., Lai, C. Y., Liao, S. L., Lu, H. C., & Chen, C. J. (2011). Luteolin inhibits cytokine expression in endotoxin/cytokine-stimulated microglia. The Journal of nutritional biochemistry, 22(7), 612–624. https://doi.org/10.1016/j.jnutbio.2010.01.011
- Weng, Zuyi et al. “Luteolin inhibits human keratinocyte activation and decreases NF-κB induction that is increased in psoriatic skin.” PloS one vol. 9,2 e90739. 28 Feb. 2014, doi:10.1371/journal.pone.0090739
- Guo, Ying-Fang et al. “Luteolin reduces inflammation in Staphylococcus aureus-induced mastitis by inhibiting NF-kB activation and MMPs expression.” Oncotarget vol. 8,17 (2017): 28481-28493. doi:10.18632/oncotarget.16092
- Törmäkangas, L., Vuorela, P., Saario, E., Leinonen, M., Saikku, P., & Vuorela, H. (2005). In vivo treatment of acute Chlamydia pneumoniae infection with the flavonoids quercetin and luteolin and an alkyl gallate, octyl gallate, in a mouse model. Biochemical pharmacology, 70(8), 1222–1230. https://doi.org/10.1016/j.bcp.2005.07.012
- Lin, T. Y., Lu, C. W., & Wang, S. J. (2016). Luteolin protects the hippocampus against neuron impairments induced by kainic acid in rats. Neurotoxicology, 55, 48–57. https://doi.org/10.1016/j.neuro.2016.05.008
- Lin, L. F., Chiu, S. P., Wu, M. J., Chen, P. Y., & Yen, J. H. (2012). Luteolin induces microRNA-132 expression and modulates neurite outgrowth in PC12 cells. PloS one, 7(8), e43304. https://doi.org/10.1371/journal.pone.0043304
- Lin, C. W., Wu, M. J., Liu, I. Y., Su, J. D., & Yen, J. H. (2010). Neurotrophic and cytoprotective action of luteolin in PC12 cells through ERK-dependent induction of Nrf2-driven HO-1 expression. Journal of agricultural and food chemistry, 58(7), 4477–4486. https://doi.org/10.1021/jf904061x
- Iakovleva, I., Begum, A., Pokrzywa, M., Walfridsson, M., Sauer-Eriksson, A. E., & Olofsson, A. (2015). The flavonoid luteolin, but not luteolin-7-O-glucoside, prevents a transthyretin mediated toxic response. PloS one, 10(5), e0128222. https://doi.org/10.1371/journal.pone.0128222
- Dirscherl, K., Karlstetter, M., Ebert, S., Kraus, D., Hlawatsch, J., Walczak, Y., Moehle, C., Fuchshofer, R., & Langmann, T. (2010). Luteolin triggers global changes in the microglial transcriptome leading to a unique anti-inflammatory and neuroprotective phenotype. Journal of neuroinflammation, 7, 3. https://doi.org/10.1186/1742-2094-7-3
- Wang, Huimin et al. “Ameliorating effect of luteolin on memory impairment in an Alzheimer's disease model.” Molecular medicine reports vol. 13,5 (2016): 4215-20. doi:10.3892/mmr.2016.5052
- Yu, T. X., Zhang, P., Guan, Y., Wang, M., & Zhen, M. Q. (2015). Protective effects of luteolin against cognitive impairment induced by infusion of Aβ peptide in rats. International journal of clinical and experimental pathology, 8(6), 6740–6747.
- Fu, X., Zhang, J., Guo, L., Xu, Y., Sun, L., Wang, S., Feng, Y., Gou, L., Zhang, L., & Liu, Y. (2014). Protective role of luteolin against cognitive dysfunction induced by chronic cerebral hypoperfusion in rats. Pharmacology, biochemistry, and behavior, 126, 122–130. https://doi.org/10.1016/j.pbb.2014.09.005
- Zhang, J. X., Xing, J. G., Wang, L. L., Jiang, H. L., Guo, S. L., & Liu, R. (2017). Luteolin Inhibits Fibrillary β-Amyloid1-40-Induced Inflammation in a Human Blood-Brain Barrier Model by Suppressing the p38 MAPK-Mediated NF-κB Signaling Pathways. Molecules (Basel, Switzerland), 22(3), 334. https://doi.org/10.3390/molecules22030334
- Kwon Y. (2017). Luteolin as a potential preventive and therapeutic candidate for Alzheimer's disease. Experimental gerontology, 95, 39–43. https://doi.org/10.1016/j.exger.2017.05.014
- Ishisaka, M., Kakefuda, K., Yamauchi, M., Tsuruma, K., Shimazawa, M., Tsuruta, A., & Hara, H. (2011). Luteolin shows an antidepressant-like effect via suppressing endoplasmic reticulum stress. Biological & pharmaceutical bulletin, 34(9), 1481–1486. https://doi.org/10.1248/bpb.34.1481
- de la Peña, J. B., Kim, C. A., Lee, H. L., Yoon, S. Y., Kim, H. J., Hong, E. Y., Kim, G. H., Ryu, J. H., Lee, Y. S., Kim, K. M., & Cheong, J. H. (2014). Luteolin mediates the antidepressant-like effects of Cirsium japonicum in mice, possibly through modulation of the GABAA receptor. Archives of pharmacal research, 37(2), 263–269. https://doi.org/10.1007/s12272-013-0229-9
- Hritcu, L., Ionita, R., Postu, P. A., Gupta, G. K., Turkez, H., Lima, T. C., Carvalho, C., & de Sousa, D. P. (2017). Antidepressant Flavonoids and Their Relationship with Oxidative Stress. Oxidative medicine and cellular longevity, 2017, 5762172. https://doi.org/10.1155/2017/5762172
- Patil, S. P., Jain, P. D., Sancheti, J. S., Ghumatkar, P. J., Tambe, R., & Sathaye, S. (2014). RETRACTED: Neuroprotective and neurotrophic effects of Apigenin and Luteolin in MPTP induced parkinsonism in mice. Neuropharmacology, 86, 192–202. https://doi.org/10.1016/j.neuropharm.2014.07.012
- Xu, J., Wang, H., Ding, K., Zhang, L., Wang, C., Li, T., Wei, W., & Lu, X. (2014). Luteolin provides neuroprotection in models of traumatic brain injury via the Nrf2-ARE pathway. Free radical biology & medicine, 71, 186–195. https://doi.org/10.1016/j.freeradbiomed.2014.03.009
- Xu, J., Wang, H., Lu, X., Ding, K., Zhang, L., He, J., Wei, W., & Wu, Y. (2014). Posttraumatic administration of luteolin protects mice from traumatic brain injury: implication of autophagy and inflammation. Brain research, 1582, 237–246. https://doi.org/10.1016/j.brainres.2014.07.042
- Theoharides T. C. (2009). Luteolin as a therapeutic option for multiple sclerosis. Journal of neuroinflammation, 6, 29. https://doi.org/10.1186/1742-2094-6-29
- Fang, J., Zhou, Q., Shi, X. L., & Jiang, B. H. (2007). Luteolin inhibits insulin-like growth factor 1 receptor signaling in prostate cancer cells. Carcinogenesis, 28(3), 713–723. https://doi.org/10.1093/carcin/bgl189
- Cook, M. T., Liang, Y., Besch-Williford, C., & Hyder, S. M. (2016). Luteolin inhibits lung metastasis, cell migration, and viability of triple-negative breast cancer cells. Breast cancer (Dove Medical Press), 9, 9–19. https://doi.org/10.2147/BCTT.S124860
- Lin, D., Kuang, G., Wan, J., Zhang, X., Li, H., Gong, X., & Li, H. (2017). Luteolin suppresses the metastasis of triple-negative breast cancer by reversing epithelial-to-mesenchymal transition via downregulation of β-catenin expression. Oncology reports, 37(2), 895–902.
- Chiang, C. T., Way, T. D., & Lin, J. K. (2007). Sensitizing HER2-overexpressing cancer cells to luteolin-induced apoptosis through suppressing p21(WAF1/CIP1) expression with rapamycin. Molecular cancer therapeutics, 6(7), 2127–2138. https://doi.org/10.1158/1535-7163.MCT-07-0107
- Kim, J. H., Lee, E. O., Lee, H. J., Ku, J. S., Lee, M. H., Yang, D. C., & Kim, S. H. (2007). Caspase activation and extracellular signal-regulated kinase/Akt inhibition were involved in luteolin-induced apoptosis in Lewis lung carcinoma cells. Annals of the New York Academy of Sciences, 1095, 598–611. https://doi.org/10.1196/annals.1397.102_2
- Zang, M. D., Hu, L., Fan, Z. Y., Wang, H. X., Zhu, Z. L., Cao, S., Wu, X. Y., Li, J. F., Su, L. P., Li, C., Zhu, Z. G., Yan, M., & Liu, B. Y. (2017). Luteolin suppresses gastric cancer progression by reversing epithelial-mesenchymal transition via suppression of the Notch signaling pathway. Journal of translational medicine, 15(1), 52. https://doi.org/10.1186/s12967-017-1151-6
- Lu, J., Li, G., He, K., Jiang, W., Xu, C., Li, Z., Wang, H., Wang, W., Wang, H., Teng, X., & Teng, L. (2015). Luteolin exerts a marked antitumor effect in cMet-overexpressing patient-derived tumor xenograft models of gastric cancer. Journal of translational medicine, 13, 42. https://doi.org/10.1186/s12967-015-0398-z
- Manju, V., & Nalini, N. (2007). Protective role of luteolin in 1,2-dimethylhydrazine induced experimental colon carcinogenesis. Cell biochemistry and function, 25(2), 189–194. https://doi.org/10.1002/cbf.1305
- Wang, H., Luo, Y., Qiao, T., Wu, Z., & Huang, Z. (2018). Luteolin sensitizes the antitumor effect of cisplatin in drug-resistant ovarian cancer via induction of apoptosis and inhibition of cell migration and invasion. Journal of ovarian research, 11(1), 93. https://doi.org/10.1186/s13048-018-0468-y
- Selvendiran, K., Koga, H., Ueno, T., Yoshida, T., Maeyama, M., Torimura, T., Yano, H., Kojiro, M., & Sata, M. (2006). Luteolin promotes degradation in signal transducer and activator of transcription 3 in human hepatoma cells: an implication for the antitumor potential of flavonoids. Cancer research, 66(9), 4826–4834. https://doi.org/10.1158/0008-5472.CAN-05-4062
- Selvendiran, K., Koga, H., Ueno, T., Yoshida, T., Maeyama, M., Torimura, T., Yano, H., Kojiro, M., & Sata, M. (2006). Luteolin promotes degradation in signal transducer and activator of transcription 3 in human hepatoma cells: an implication for the antitumor potential of flavonoids. Cancer research, 66(9), 4826–4834. https://doi.org/10.1158/0008-5472.CAN-05-4062
- Yi, C., Li, G., Ivanov, D. N., Wang, Z., Velasco, M. X., Hernández, G., Kaundal, S., Villarreal, J., Gupta, Y. K., Qiao, M., Hubert, C. G., Hart, M. J., & Penalva, L. (2018). Luteolin inhibits Musashi1 binding to RNA and disrupts cancer phenotypes in glioblastoma cells. RNA biology, 15(11), 1420–1432. https://doi.org/10.1080/15476286.2018.1539607
- Cook, M. T., Liang, Y., Besch-Williford, C., & Hyder, S. M. (2016). Luteolin inhibits lung metastasis, cell migration, and viability of triple-negative breast cancer cells. Breast cancer (Dove Medical Press), 9, 9–19. https://doi.org/10.2147/BCTT.S124860
- Wang, H., Luo, Y., Qiao, T., Wu, Z., & Huang, Z. (2018). Luteolin sensitizes the antitumor effect of cisplatin in drug-resistant ovarian cancer via induction of apoptosis and inhibition of cell migration and invasion. Journal of ovarian research, 11(1), 93. https://doi.org/10.1186/s13048-018-0468-y
- Shi, R., Huang, Q., Zhu, X., Ong, Y. B., Zhao, B., Lu, J., Ong, C. N., & Shen, H. M. (2007). Luteolin sensitizes the anticancer effect of cisplatin via c-Jun NH2-terminal kinase-mediated p53 phosphorylation and stabilization. Molecular cancer therapeutics, 6(4), 1338–1347. https://doi.org/10.1158/1535-7163.MCT-06-0638
- Lin, Y., Shi, R., Wang, X., & Shen, H. M. (2008). Luteolin, a flavonoid with potential for cancer prevention and therapy. Current cancer drug targets, 8(7), 634–646. https://doi.org/10.2174/156800908786241050
- Wang, X., & Quinn, P. J. (2010). Endotoxins: lipopolysaccharides of gram-negative bacteria. Sub-cellular biochemistry, 53, 3–25. https://doi.org/10.1007/978-90-481-9078-2_1
- Xagorari, A., Papapetropoulos, A., Mauromatis, A., Economou, M., Fotsis, T., & Roussos, C. (2001). Luteolin inhibits an endotoxin-stimulated phosphorylation cascade and proinflammatory cytokine production in macrophages. The Journal of pharmacology and experimental therapeutics, 296(1), 181–187.
- Kumazawa, Y., Kawaguchi, K., & Takimoto, H. (2006). Immunomodulating effects of flavonoids on acute and chronic inflammatory responses caused by tumor necrosis factor alpha. Current pharmaceutical design, 12(32), 4271–4279. https://doi.org/10.2174/138161206778743565
- Kotanidou, A., Xagorari, A., Bagli, E., Kitsanta, P., Fotsis, T., Papapetropoulos, A., & Roussos, C. (2002). Luteolin reduces lipopolysaccharide-induced lethal toxicity and expression of proinflammatory molecules in mice. American journal of respiratory and critical care medicine, 165(6), 818–823. https://doi.org/10.1164/ajrccm.165.6.2101049
- Xagorari, A., Roussos, C., & Papapetropoulos, A. (2002). Inhibition of LPS-stimulated pathways in macrophages by the flavonoid luteolin. British journal of pharmacology, 136(7), 1058–1064. https://doi.org/10.1038/sj.bjp.0704803
- Chen, C. Y., Peng, W. H., Tsai, K. D., & Hsu, S. L. (2007). Luteolin suppresses inflammation-associated gene expression by blocking NF-kappaB and AP-1 activation pathway in mouse alveolar macrophages. Life sciences, 81(23-24), 1602–1614. https://doi.org/10.1016/j.lfs.2007.09.028
- Wu, C. C., Fang, C. Y., Hsu, H. Y., Chen, Y. J., Chou, S. P., Huang, S. Y., Cheng, Y. J., Lin, S. F., Chang, Y., Tsai, C. H., & Chen, J. Y. (2016). Luteolin inhibits Epstein-Barr virus lytic reactivation by repressing the promoter activities of immediate-early genes. Antiviral research, 132, 99–110. https://doi.org/10.1016/j.antiviral.2016.05.007
- Wu, C. C., Fang, C. Y., Hsu, H. Y., Chuang, H. Y., Cheng, Y. J., Chen, Y. J., Chou, S. P., Huang, S. Y., Lin, S. F., Chang, Y., Tsai, C. H., & Chen, J. Y. (2016). EBV reactivation as a target of luteolin to repress NPC tumorigenesis. Oncotarget, 7(14), 18999–19017. https://doi.org/10.18632/oncotarget.7967
- Bai, L., Nong, Y., Shi, Y., Liu, M., Yan, L., Shang, J., Huang, F., Lin, Y., & Tang, H. (2016). Luteolin Inhibits Hepatitis B Virus Replication through Extracellular Signal-Regulated Kinase-Mediated Down-Regulation of Hepatocyte Nuclear Factor 4α Expression. Molecular pharmaceutics, 13(2), 568–577. https://doi.org/10.1021/acs.molpharmaceut.5b00789
- Fan, W., Qian, S., Qian, P., & Li, X. (2016). Antiviral activity of luteolin against Japanese encephalitis virus. Virus research, 220, 112–116. https://doi.org/10.1016/j.virusres.2016.04.021
- Lim, S. H., Jung, S. K., Byun, S., Lee, E. J., Hwang, J. A., Seo, S. G., Kim, Y. A., Yu, J. G., Lee, K. W., & Lee, H. J. (2013). Luteolin suppresses UVB-induced photoageing by targeting JNK1 and p90 RSK2. Journal of cellular and molecular medicine, 17(5), 672–680. https://doi.org/10.1111/jcmm.12050
- Byun, S., Lee, K. W., Jung, S. K., Lee, E. J., Hwang, M. K., Lim, S. H., Bode, A. M., Lee, H. J., & Dong, Z. (2010). Luteolin inhibits protein kinase C(epsilon) and c-Src activities and UVB-induced skin cancer. Cancer research, 70(6), 2415–2423. https://doi.org/10.1158/0008-5472.CAN-09-4093
- Balunas, M. J., Su, B., Brueggemeier, R. W., & Kinghorn, A. D. (2008). Natural products as aromatase inhibitors. Anti-cancer agents in medicinal chemistry, 8(6), 646–682.
- Yahyazadeh, A., & Altunkaynak, B. Z. (2019). Protective effects of luteolin on rat testis following exposure to 900 MHz electromagnetic field. Biotechnic & histochemistry : official publication of the Biological Stain Commission, 94(4), 298–307. https://doi.org/10.1080/10520295.2019.1566568
- Nabavi, S. F., Braidy, N., Gortzi, O., Sobarzo-Sanchez, E., Daglia, M., Skalicka-Woźniak, K., & Nabavi, S. M. (2015). Luteolin as an anti-inflammatory and neuroprotective agent: A brief review. Brain research bulletin, 119(Pt A), 1–11. https://doi.org/10.1016/j.brainresbull.2015.09.002